Explore the USDA’s proposed bulk milk testing initiative designed to tackle bird flu in dairy herds ahead of cattle transport. Will this innovative method safeguard our milk supply?

In a decisive effort to safeguard the dairy industry amidst a health crisis, the U.S. Agriculture Department (USDA) has proposed bulk milk testing for bird flu before cattle transport. This strategy aims to streamline testing, offering hope to farmers grappling with the virus’s spread to cows and dairy workers. The USDA must balance rigorous disease control with economic realities as the pandemic threat looms.
“The USDA’s proposed bulk milk testing could be a transformative step, offering a more efficient method for ensuring herd health and preventing further economic fallout,” said an industry representative, emphasizing the potential positive impact of this strategy.
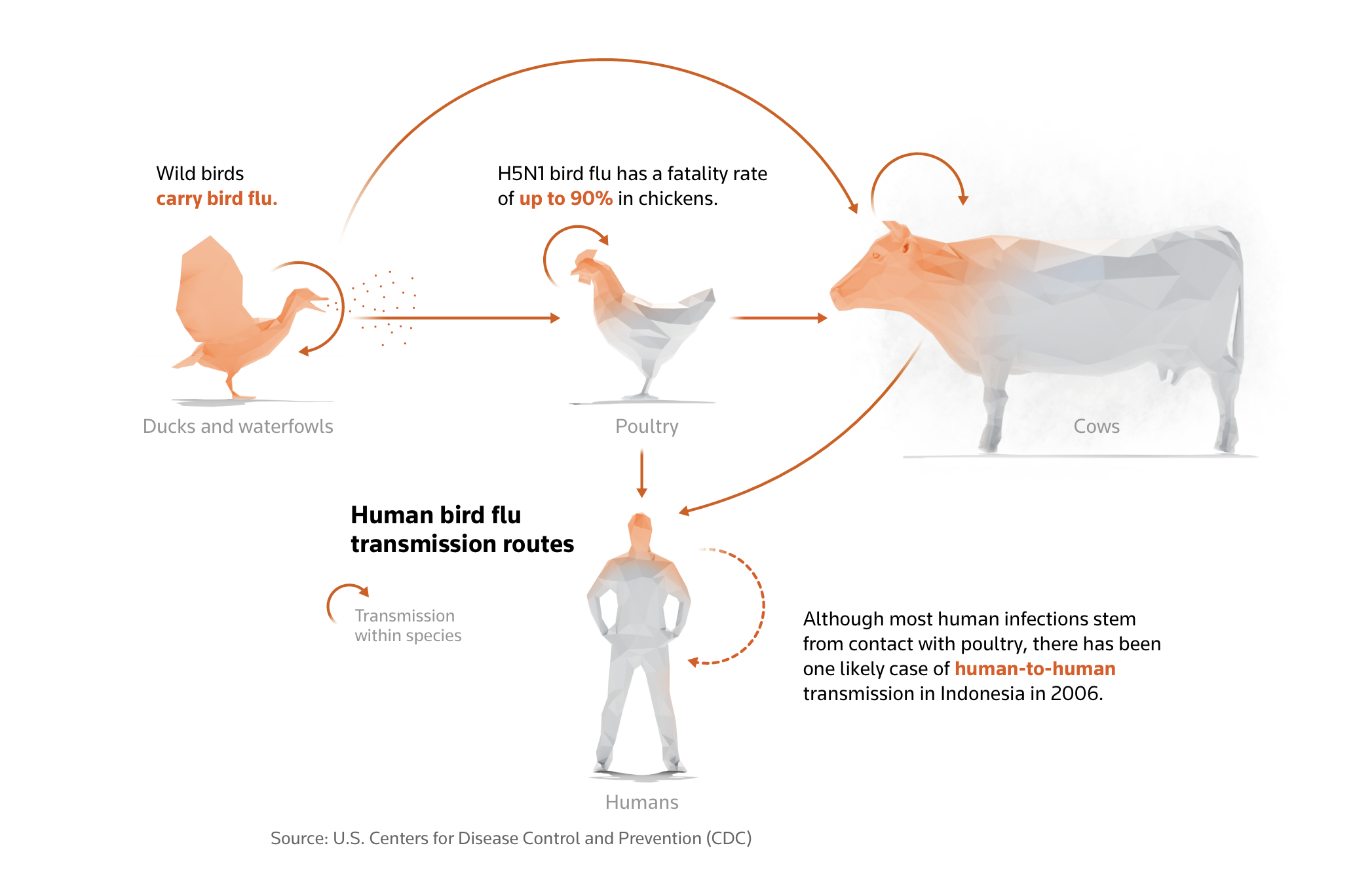
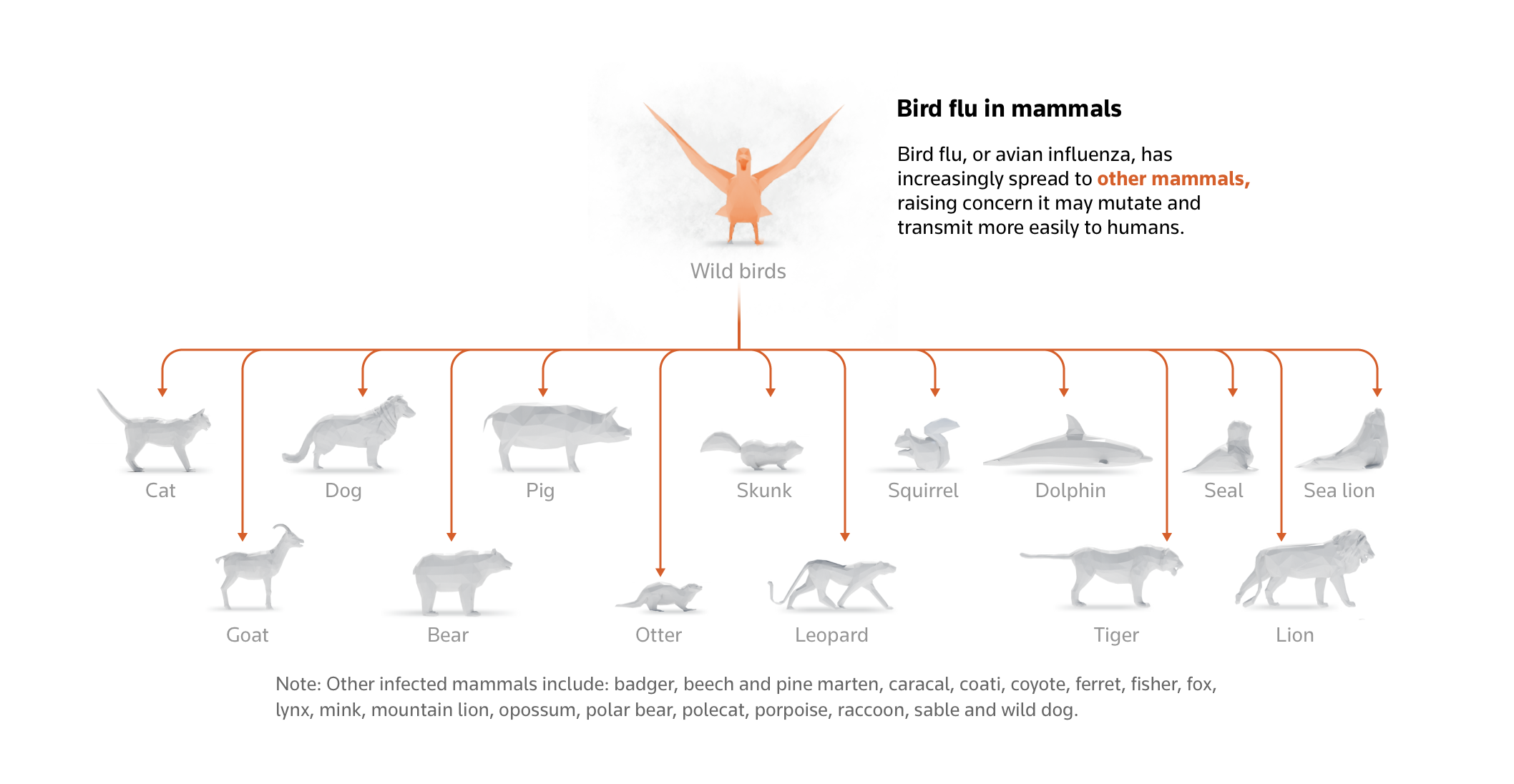
Since late March, the H5N1 bird flu virus, a highly contagious and potentially deadly strain, has crossed species barriers, infecting dairy cows and even two dairy workers. This has raised the stakes in public health and agricultural stability. As of late April, the USDA mandated negative tests for lactating cows before interstate travel, containing the virus but also imposing logistical burdens on dairy farmers.
- Bulk milk testing could significantly reduce individual animal tests, streamlining the process.
- The pilot program starts in June, allowing farmers to sample milk from bulk storage tanks.
- Efficient, collective testing is expected to mitigate health risks and economic impacts.
The USDA’s proposal to sustain the nation’s health and essential dairy industry reflects a steadfast commitment to disease containment and agricultural viability, providing stakeholders with a sense of reassurance.
Swift Measures Against Avian Flu: USDA’s Mandatory Testing for Interstate Transport
In response to the bird flu outbreak in dairy cattle, the USDA mandated in April that lactating cows test negative for H5N1 before interstate transport. This quick action was crucial in stopping the virus from spreading to new regions, preventing a potential nationwide crisis. Early enforcement of these tests has been vital in containing the virus, buying time to develop better testing and control methods.
Tracking Challenges: Discrepancies in Bulk Testing and Animal Monitoring
The USDA initiated mandatory testing for lactating cows before interstate transport to address the avian flu spread. So far, 2,492 tests have been conducted. However, this number reflects tests administered, not individual animals tested. This could obscure the number of cows monitored, complicating tracking and containment efforts.
Pioneering New Frontiers: USDA’s Novel Pilot Program for Bulk Milk Testing
The USDA’s proposed pilot program for bulk milk testing marks a strategic pivot towards more efficient disease control in dairy herds. Set to begin in June; this voluntary program will allow farmers to test milk from bulk storage tanks, thereby sampling the collective output of all cows in a herd and reducing the labor-intensive individual testing process.
The program requires bulk tanks from herds to show three consecutive weeks of negative results to establish a herd’s freedom from bird flu. Once confirmed, farmers must submit weekly milk samples to maintain this status, eliminating the need for further testing before interstate transport, provided the herds continue to test negative.
The USDA believes that sufficient farmer participation in the bulk milk testing program could help establish disease-free zones in states or regions, curb the spread of H5N1, protect farm workers, and safeguard the commercial milk supply. However, the adequacy of the testing method and logistical challenges, such as the need for proper equipment and training, remain key concerns among stakeholders.
Mixed Reactions from State Officials and Industry Leaders on USDA’s Bulk Milk Testing Proposal
State agriculture officials and industry leaders have reacted variably to the USDA’s bulk milk testing proposal. Officials from six states are examining the program, with differing levels of interest and apprehension. Tim Boring of Michigan’s Department of Agriculture noted the need to limit animal movement to curb the spread of the disease. Still, it showed keen interest given Michigan’s high infection rates. Conversely, Indiana’s state veterinarian, Bret Marsh, voiced concerns about the program’s market implications and the potential for increased restrictions on local producers.
The International Dairy Foods Association backed the initiative on the industry side, underscoring its potential to lower H5N1 risks in dairy herds, protect farm workers, and secure the commercial milk supply. With adequate farm participation, they believe the USDA’s program could greatly enhance disease control.
Rising Pandemic Threat: The Alarming Spread of H5N1 Bird Flu in U.S. Dairy Industry
The H5N1 bird flu virus, known for its rapid mutation and cross-species infection, has deeply infiltrated the U.S. dairy cattle sector. Outbreaks confirmed in nine states highlight how livestock movement spreads the virus. The FDA’s alarming estimate shows that about 20% of the U.S. milk supply is now contaminated. This underscores H5N1’s reach and signals potential economic and public health risks from contaminated dairy products.
Streamlining Dairy Operations: Farmers Endorse Bulk Milk Testing as a Practical Solution to Combat Bird Flu
Many farmers see bulk milk testing from storage tanks as a more efficient alternative to testing each cow individually. Collecting a sample from an entire herd simultaneously streamlines the process. It saves time, allowing farms to meet regulatory requirements without disrupting daily operations. As one farmer said, “Testing each cow individually is not only time-consuming but also impractical, especially for large herds.”
The USDA’s requirements for maintaining a disease-free status under the pilot program are stringent. Bulk tanks of milk must test negative for three consecutive weeks before qualifying. Once approved, weekly samples are mandatory to avoid additional testing before interstate cattle transport. If enough farmers participate, disease freedom could be declared in specific states, easing animal movement. However, a single positive result would prompt a thorough epidemiologic investigation, highlighting the high stakes of maintaining disease-free status and the crucial role of stakeholders in this process.
Weighing the Pros and Cons: Bulk Milk Testing’s Efficiency and Its Pitfalls
The proposed USDA bulk milk testing program offers significant advantages for large dairies. By testing milk from bulk storage tanks instead of individual cows, farmers can manage herds more efficiently, saving time and resources. This streamlined method could expedite the approval process for transporting cattle across state lines, ensuring supply chain continuity and reducing the virus’s spread to new regions. Weekly milk sample submissions may help dairy operations quickly identify and isolate outbreaks, mitigating risks to both livestock and workers.
However, it’s important to address concerns raised by experts like veterinary and public health consultant Gail Hansen about the reliability of bulk testing in detecting infections. Hansen argues that milk from healthy cows could dilute samples from infected animals, potentially leading to false negatives. The USDA acknowledges these concerns and is committed to a thorough evaluation of the bulk milk testing method to ensure its accuracy and effectiveness in detecting the virus.
Interstate Impediments: Indiana and Texas Officials Raise Alarms Over USDA’s Bulk Milk Testing Protocols
Bret Marsh, Indiana’s state veterinarian, spotlighted logistical issues with the proposed bulk milk testing. A key concern is that Indiana could be labeled an “affected state” if positive test results emerge. This would lead to strict restrictions and challenging interstate cattle movement, complicating market conditions for local farmers.
Texas representatives noted that despite being informed by the USDA about the initiative, crucial implementation details still need to be included. This lack of clarity leaves state officials needing to be made aware of the program’s practical enforcement. These ambiguities could impede the program’s acceptance and execution, requiring the USDA to offer a more transparent framework before launch.
Diverse State Stances: Texas Seeks Clarity, Indiana Voices Concerns and Michigan Takes Proactive Measures
Texas is aware of the USDA’s proposed bulk milk testing program but seeks clarification on implementation details, emphasizing the need for a thorough understanding before committing.
Indiana, led by state veterinarian Bret Marsh, has concerns about the implications of gathered data. They fear infection findings could classify Indiana as an affected state, leading to stricter restrictions from neighboring states and disadvantaging Hoosier farmers.
Michigan, facing the highest number of confirmed cattle infections, takes a proactive stance under Tim Boring’s direction at the Department of Agriculture and Rural Development. Boring supports restricting animal movement to prevent the spread of H5N1, aiming to keep sick cattle from spreading the virus across farms.
The Bottom Line
The USDA’s proposal for bulk milk testing before cattle transport aims to balance disease control with economic efficiency. Reactions are mixed: some view it as essential for public health and the national milk supply, while others worry about the logistics, effectiveness, and market impact. This highlights the complexity of managing a pandemic threat in agriculture.
Ongoing testing, surveillance, and investigations emphasize the USDA’s dedication to reducing risks while limiting economic harm to farmers.
Key Takeaways:
- The USDA has confirmed H5N1 bird flu in cattle across nine states, and 20% of the U.S. milk supply shows signs of the virus.
- The proposed bulk testing program aims to reduce individual animal tests, with weekly samples needed to maintain disease-free status.
- State officials have raised concerns over the program’s logistics and potential market implications.
- Pilot bulk milk testing is set to begin in June, with varied reactions from states like Indiana, Texas, and Michigan.








 Picture an hour spent in a warm embrace with a friendly cow, an hour where worries dissolve and serenity overtakes. Now imagine this act of sweetness could actually be contributing to a cause, paying for a bale of hay that, in turn, provides nourishment for the very cattle you’re cuddling. A delightful scenario, right? But there’s a catch. Unfortunately, this trend, popularized on social media, might be hanging in the balance due to a recent outbreak of avian influenza detected among
Picture an hour spent in a warm embrace with a friendly cow, an hour where worries dissolve and serenity overtakes. Now imagine this act of sweetness could actually be contributing to a cause, paying for a bale of hay that, in turn, provides nourishment for the very cattle you’re cuddling. A delightful scenario, right? But there’s a catch. Unfortunately, this trend, popularized on social media, might be hanging in the balance due to a recent outbreak of avian influenza detected among  Could avian influenza jump species and infect cows globally? Explore the potential international impact of this unprecedented event in our in-depth analysis.
Could avian influenza jump species and infect cows globally? Explore the potential international impact of this unprecedented event in our in-depth analysis. Discover the latest updates on the US’s proactive measures to test ground beef amid bird flu outbreaks in dairy cows. Will your state be affected? Find out now.
Discover the latest updates on the US’s proactive measures to test ground beef amid bird flu outbreaks in dairy cows. Will your state be affected? Find out now. Discover why dairy farmers hesitate to report potential avian flu cases. Uncover the reality behind this reluctance and join the conversation for change.
Discover why dairy farmers hesitate to report potential avian flu cases. Uncover the reality behind this reluctance and join the conversation for change.



